Mental Wellbeing and Resilience of Immigrants in Facing Emerging Social Crises
Bienestar psicológico y resiliencia de los inmigrantes
en crisis sociales emergentes
Héctor Cebolla Boado and Álvaro Suárez-Vergne
|
Key words
Immigration
- Mental Wellbeing
- Global Health Questionnaire-12
- Lockdown
- COVID-19
- Economic Vulnerability
- Support Networks
- Healthy Immigrant Paradox
|
Abstract
This study compares the psychological impact experienced by immigrants and natives during the spring 2020 lockdowns in Madrid (Spain). We utilize data from the Spanish 2017 National Health Survey, and the Madrid Covid Household Panel. Overall, the population at risk of psychological morbidity peaked at around 60 % during the lockdowns. The behaviour of immigrants and natives is strikingly similar. However, a single dimension emerges in which immigrants are notably more psychologically vulnerable. The reduction in income imposed a greater loss of mental wellbeing on immigrants than on natives. Thus, the evidence provided highlights an immigrant population which registers similar levels of distress as natives, but the greater economic vulnerability faced by immigrants exposes them to greater distress. These findings can inform public policies during future health crises.
|
|
Palabras clave
Inmigración
- Bienestar psicológico
- Cuestionario Global de Salud-12
- Confinamiento
- COVID-19
- Vulnerabilidad económica
- Redes de apoyo
- Paradoja del inmigrante saludable
|
Resumen
En este artículo se compara el bienestar psicológico de inmigrantes y nativos durante los confinamientos de la primavera de 2020 en Madrid (España). Se utilizan datos de la Encuesta Nacional de Salud de 2017, y del Panel de Hogares de COVID-19 de Madrid. En general, la población en riesgo de morbilidad psicológica llega al 60 % durante los confinamientos. No se encuentran grandes diferencias entre inmigrantes ni nativos. Sin embargo, la reducción de ingresos tiene un mayor impacto psicológico en los inmigrantes. La evidencia proporcionada destaca una población migrante que registra niveles de bienestar psicológico idénticos a los de los nativos. Sin embargo, la vulnerabilidad económica que enfrentan los migrantes los expone a un mayor malestar. Estos resultados pueden contribuir a la elaboración de políticas públicas en futuras crisis sanitarias.
|
Citation
Cebolla Boado, Héctor; Suárez-Vergne, Álvaro (2025). “Mental Wellbeing and Resilience of Immigrants in Facing Emerging Social Crises”. Revista Española de Investigaciones Sociológicas, 190: 89-110. (doi: 10.5477/cis/reis.190.89-110)
Héctor Cebolla Boado: Instituto de Economía, Geografía y Demografía (IEGD) – CSIC | hector.cebolla@cchs.csic.es
Álvaro Suárez-Vergne (corresponding author): Instituto de Economía, Geografía y Demografía (IEGD) – CSIC | alvaro.suarez@cchs.csic.es
Introduction
The social sciences are struggling to analyse the extensive consequences of COVID-19 beyond mortality (Ngo and Psaki, 2021). Among these, its influence on migration could have a lasting and profound effect due to the normalization of border closures and travel restrictions, which has further underscored the vulnerability of immigrants (Merchant, 2021). This is precisely the prospect our study aims to address, as we uncover patterns of psychological vulnerability among immigrant groups of different status amid mobility constraints.
Mainstream research on integration has traditionally prioritized measurable outcomes, including labour market performance and education. Yet, most of these results are significantly influenced by certain subjective factors that often go unnoticed in integration research. While the prominence of research on mental wellbeing in vulnerability studies is on the rise (Brady, 2019), its recognition within the realm of integration is only gradually gaining traction. Numerous studies have pinpointed subjective, “soft” and intricately measurable dimensions of wellbeing as prerequisites for establishing a level playing field for all individuals to compete equitably. Among these, one of the least explored, yet potentially pivotal, is mental wellbeing. While there is a large tradition of measuring psychological wellbeing in epidemiological studies, appropriate measurement tools (Kessler et al., 2002; Griffith and Jones, 2019) are frequently absent in mainstream surveys. This explains why, in most cases, subjective wellbeing is often proxied through self-reported indicators such as happiness, optimism, and self-confidence (Hendriks and Bartram, 2019; Bak-Klimek et al., 2015).
Migration entails exposure to intense stressors, including uprooting and severing ties with homeland networks, risks inherent in the journey, discrimination upon arrival, and cultural dissonance between place of origin and destination. This predisposes immigrants to enduring vulnerability (Choy et al., 2021) and often overlooked challenges in achieving status convergence with natives. For some, immigration involves a form of ‘grief’ and is a genuine risk factor for mental wellbeing that can resurface deeply ingrained traumas from the past, amplify their impact and give rise to ambivalent emotions that reach not only the immigrant but also those left behind (Achotegui, 2009). By exploring the intersection between immigration and mental wellbeing, our study makes three significant contributions to the research agenda on immigrant integration. First, it addresses a frequently overlooked soft dependent variable in demographic research by investigating how immigrants emotionally navigate daily life difficulties and external shocks. Secondly, our research paves the way for uncovering hidden factors that might affect immigrants and natives differently, potentially making immigrants more psychologically vulnerable to unforeseen stressors and ultimately more disadvantaged in measurable outcomes of integration. Lastly, we provide valuable insights from Spain.
Despite having hosted substantial migration flows in recent decades, the country remains a rare case in epidemiological research on immigration and mental wellbeing. Public health policies during times of crisis may have a protective effect on the health of vulnerable groups such as immigrants (Endale et al., 2020; Doan et al., 2021); we believe that studies such as ours can contribute to generating information specifically focused on the Spanish context. This information could be valuable for developing public policies aimed at safeguarding the health of immigrant groups.
The mental wellbeing
of immigrants in advanced economies
At the risk of oversimplifying complex theoretical and empirical traditions, epidemiological research on mental wellbeing and immigrant status has generated two main currents of reflection. First, almost a century ago pioneering studies on the mental health of immigrants identified their greater likelihood of suffering from certain conditions such as psychosis, something that would shortly be explained by the selection bias involved in migration (Odegaard, 1932). The most reliable meta-reviews suggest that, indeed, immigrant status seems to be associated with a certain decline in mental wellbeing due to the harsh economic restrictions faced by most economic immigrants and the lack of support networks (Hasan et al., 2021). However, no consensus has yet been reached on this regard. Part of the literature argues that immigration involves an increased risk of mental illness (He and Wong, 2013; Breslau, 2011; Maggi et al., 2010; Adhikari, Jampaklay, and Chamratrithirong, 2011; Banal et al., 2010), although the danger of over-diagnosing and essentializing this potential immigrant vulnerability has been noted (Achotegui, 2017). In contrast, other studies have found no relationship between immigration and mental wellbeing (Mood, Jonsson, and Låftman, 2016; Stillman, Gibson, and McKenzie, 2012). While research on Spain is still limited, some studies have documented some disadvantage in mental wellbeing (Jarrín et al., 2013; Plaza et al., 2005) related to factors such as stepwise family migration (Cebolla-Boado and González-Ferrer, 2022) and spatial concentration (Cebolla-Boado and Aratani, 2020).
Secondly, research on the mental health and wellbeing of immigrants has also discussed the “healthy immigrant paradox”, which accounts for the unexpected better (mental) health (Rivera, Casal, and Currais, 2016; Elshahat, Moffat, and Newbold, 2022; Dhadda and Greene, 2018) of economic immigrants given their generally worse than average position in the social stratification system (Teruya and Bazargan-Hejazi, 2013; Riosmena, Kuhn, and Jochem, 2017). This “paradox” was initially documented in the United States but has been confirmed in European countries. The debate has focused on two central axes, on the one hand, documenting whether this advantage remains stable over time (Antecol and Bedard, 2006) and, on the other, identifying the causes of this advantage, which range from statistical artifacts due to positive self-selection involved in migration in terms of physical and mental strength (Elshahat, Moffat, and Newbold, 2021; Dhadda and Greene, 2018), and negative selection among returnees to countries of origin, a phenomenon known as the “salmon bias” (Turra and Elo, 2008).
From this summary of the relevant literature, we draw two main initial hypotheses:
H1: Immigrant emotional vulnerability: The adversities migrants face while striving for optimal integration outcomes may also emotionally disadvantage them, resulting in lower levels of mental wellbeing compared to natives.
H2: Healthy immigrant effect: We expect migrants to exhibit greater resilience than comparable natives and, therefore, report higher levels of mental wellbeing even in harsh circumstances.
The pandemic turned a large part of the planet into a laboratory for the study of the cost of the confinement measures that were applied with greater or lesser intensity in many countries. This has prompted the interest of sociologists, demographers, economists, and epidemiologists in systematizing the social and contextual factors that determine the mental wellbeing of populations. In addition, studies on the integration of immigrants have also received a push in this direction. While not an exhaustive review of the current research agenda in this area, we can point to some recent findings. Lockdowns reduced subjective life satisfaction and mental wellbeing among the immigrant population (Ekwonye, Ezumah, and Nwosisi, 2021; Garrido et al., 2023), making those who were already in a worse relative position more vulnerable (Acharya et al., 2022). Shen and Bartran (2021) have shown that the disruption of labour trajectories has not had as negative an effect on the mental wellbeing of natives as on that of immigrants, particularly among males who have reduced their labour intensity and earnings more. Everything seems to indicate that the greater psychological cost has been borne, above all, by those who were already in an irregular situation (Enriquez et al., 2022), as well as by those who suffered job insecurity, family stress and more acute information deficits (Garcini et al., 2022). Finally, this worsening of subjective wellbeing may have also increased perceptions of barriers between minority groups and the majority: an “us” versus “them” discourse (Arora et al., 2022).
Our study delves deeper to uncover whether other additional stressors contributed to further weaken the emotional stability of immigrants in Spain. First, the financial instability that most economic immigrants encounter, particularly during their initial years of residence or until they become regular residents and accumulate country-specific human capital, can make their mental wellbeing more sensitive to shrinking levels of income and economic insecurity. Immigrants are likely to have less savings to face unexpected events (Bover, Hospido, and Villanueva, 2018; Sarasa, Navarro-Varas, and Porcel, 2016) and face high costs until settled (Agius and Keister, 2020). Furthermore, remittances and the responsibility immigrants often have in ensuring the wellbeing of their relatives left behind, may further amplify the impact of economic insecurity among immigrants compared to natives. This leads us to draw an additional hypothesis:
H3: Economic vulnerability: The mental wellbeing of migrants may be more sensitive to experiencing a decrease in earnings due to shifting labour conditions.
Secondly, restricted access to or limited understanding of the health system may have resulted in a more significant loss of wellbeing in immigrant households with infected cohabiting members. While access to healthcare in Spain is universal for all locally registered residents, including undocumented persons, it has been shown that recent, and particularly undocumented, immigrants are much less likely to formalize their registration (Hacker et al., 2015), which undoubtedly complicates their contact with the public health care system. This leads to our fourth hypothesis:
H4: Access to healthcare: Direct exposure to COVID in the household leading to the isolation of relatives or coresidents in the household or suspicion of being infected may have had a more detrimental impact on the mental wellbeing of migrants compared to that of natives, whose access to healthcare is more normalized.
Finally, according to reliable meta-reviews, feeling connected and supported by others alleviates the harshness of immigration (Bak-Klimek et al., 2015). It is generally known that immigrants’ support networks are smaller compared to those of natives (Kindler, Ratcheva, and Piechowska, 2015). Immigrants may have encountered deteriorating relationships more damaging to their psychological wellbeing than natives precisely because of weak support networks (Salinero-Fort et al., 2011; Jariego, 2009). This can make immigrants more vulnerable to a worsening atmosphere at home, ultimately affecting their mental wellbeing more. This leads to our fifth and last hypothesis:
H5: Support network: The mental wellbeing of migrants may be more sensitive to a worsening household atmosphere compared to that of natives due to their smaller support networks.
Methodology
Datasets
In this study we used two different datasets. Our main source is the “Madrid Covid Household Panel”, the first wave of which was conducted by the Madrid City Council in April 2020, with a follow-up in October 2020. The Panel is a unique tool for this kind of research not only because it included well-stablished measures of mental wellbeing in epidemiological research (see below), but also because of the context of the survey. During the initial wave of the pandemic, Spain arguably endured some of the most stringent lockdown measures in Europe. These measures had profound repercussions on the labour market, a fact that has already been extensively documented as a source of significant stressors (Escudero-Castillo, Mato-Díaz and Rodríguez-Alvarez, 2023). This survey provides a unique opportunity to document how natives and foreign-born reacted to persistent difficulties to maintain their daily lives and economic activities, as low-skilled jobs and interpersonal services, where a large part of the immigrant population is concentrated in the labour market, were particularly restricted.
The survey targeted all households in the city of Madrid with at least one member aged 18 or over. In the first wave, a total of 1566 valid responses were obtained using a two-stage sampling procedure in which primary sampling units (households) were selected by randomly generating telephone numbers based on quotas for gender, age, district, and household type. Given the constraints at the time, fieldwork was conducted by telephone (landline: 80.5 %; mobile: 19.5 %). Unfortunately, the second wave, which we only use for complementary analyses and robustness checks, carried out in October 2020 only recruited 957 respondents from the original sample.
As supplementary data, we used the National Health Survey (NHS) in Spain as a benchmark for comparing the mental wellbeing of immigrants and natives under normal and extraordinary circumstances. The NHS is a well-known data set used for epidemiological reference produced by Spain’s National Institute of Statistics. For the sake of comparability with our main results, we use the 2017 wave, the closest to the lockdowns, and we restrict the analytical sample to respondents in the Region of Madrid (n=2032 adults).
Measuring mental wellbeing
A well-known standardized tool in the social sciences to quantitatively assess the mental wellbeing of a population and its social determinants is the General Health Questionnaire (Williams and Goldberg, 1988). The Madrid Panel included the 12 items version (GHQ12) of this indicator. The GHQ12 is a widely used measure in many large European statistical projects, such as the British Household Panel and the Millennium Cohort. Because of its high reliability, it is commonly used to assess levels of stress in a population. However, it should be noted that there are ongoing debates about the dimensions it covers (Griffith and Jones, 2019), as it tends to overestimate mental wellbeing among males and persons facing changes in employment or socioeconomic status (Brown et al., 2018). In addition, respondents who are financially better-off and have higher social support may be false positive, in other words, incorrectly categorised as individuals with mental health problems more often than other groups (Bell et al., 2005). Nevertheless, it is commonly accepted that the GHQ12 works reasonably well as an indicator of depression and/or anxiety disorders (Lundin et al., 2016; Baksheev et al., 2011). In Spain, the subsequent unidimensional scale constructed from these 12 items for measuring mental wellbeing in the general population has been validated and found to be significantly associated with the incidence of mental disorders (Rocha et al., 2011; Rodrigo et al., 2019). The items included in this standardized epidemiological tool for quantifying mental wellbeing, and their translation into English, are given in the following table:
Table 1. Global Health Questionnaire-12
|
Have you been able to concentrate well on what you were doing?
|
|
Have your worries made you lose a lot of sleep?
|
|
Have you felt that you are playing a useful role in life?
|
|
Have you felt capable of making decisions?
|
|
Have you felt constantly overwhelmed and tense?
|
|
Have you had the feeling that you cannot overcome your difficulties?
|
|
Have you been able to enjoy your normal daily activities?
|
|
Have you been able to adequately cope with your problems?
|
|
Have you felt unhappy or depressed?
|
|
Have you lost confidence in yourself?
|
|
Have you thought that you are a worthless person?
|
|
Do you feel reasonably happy considering all the circumstances?
|
Source: GeneHealth Questionnaire, GHQ (Williams and Goldberg, 1988).
Answers were registered using a Likert scale (scored from 0 to 4: Always, Sometimes, Rarely, Never, plus a don’t know/no answer). From the responses, a synthetic indicator of mental wellbeing is usually derived, which refers to the emotional risk to which a population is exposed. Several methods for constructing such an indicator are described in the literature. Here we employ Likert scoring (Goldberg et al., 1997): summing all values according to their original scores and taking 12 as the critical threshold. Therefore, in our analyses scores below 12 are denoted as zero, meaning no psychological risk, as opposed to those scoring 12 or more, which are coded as 0, indicating a significant risk of morbidity.
Data analysis
We have carried out a stepwise hierarchical logistic regression analysis (Snijders and Bosker, 2012) on the qualitative recodification of GHQ12 (<12=0: low distress or no risk; ≥12=1: being at psychological risk) as the dependent variable of interest. Our model clusters respondents in each of the 21 districts of Madrid. Hierarchical binary logistic regressions are a conservative strategy to discard biased results due to the different incidence of COVID in the city. Indeed, the disease did not affect Madrid symmetrically across the territory but had a higher incidence in the southern and eastern districts of the city, precisely where the immigrant population is concentrated (García, 2020).
First, we allow for unconditional comparisons across migrant status in 2017 and April 2020. We then adjust our estimates controlling by sex, age, and square meters of household per capita as control variables, and education (primary or less, secondary, vocational and university graduates) to contrast whether specific groups are particularly at psychological risk. Next, we explore two-way interactions between immigrant status and three concurring stressors on mental wellbeing: 1) the impact of experiencing a decrease in earnings due to shifting labour conditions (being laid off, being affected by a temporary contract cessation, or experiencing a reduction in the number of working hours for the active population) for those working or already unemployed in April 2020; 2) the incidence of the disease in the household as proxied by living with a person isolated by Covid; and 3) a deteriorating atmosphere in the household. Table A1 in the Appendix provides descriptive information about all the variables involved in the analyses.
Results
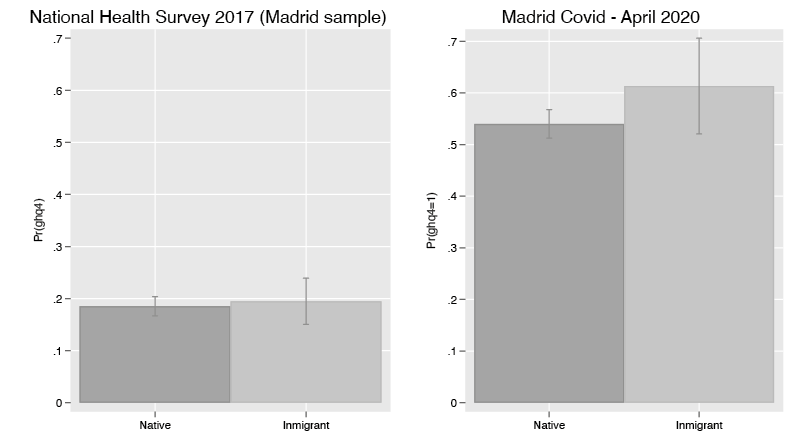
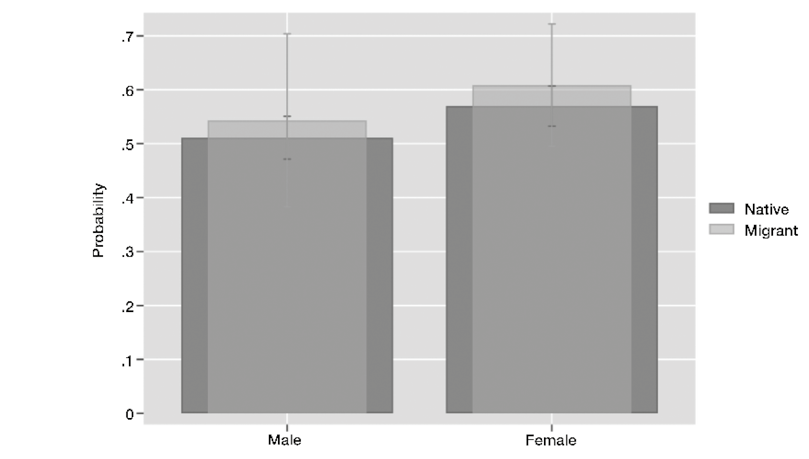
Did the lockdown affect immigrants and natives differently? How severely did the shock impact their psychological wellbeing? The bars in Graph 1 represent the proportion of the respondents whose psychological wellbeing was at risk in 2017 and during the 2020 lockdowns (Models are presented in Table A2 in the Appendix).
Two significant conclusions emerge from these descriptive analyses. First, the pandemic and subsequent lockdowns led to a profound increase in psychological distress among all respondents. Under ordinary circumstances, such as those in 2017, only 20 % of respondents gave signs of psychological distress (18.5 % of natives and 19.4 % of immigrants). However, by April 2020, this figure increased to 54.0 % for natives and 61.3 % for immigrants. To put it simply, during the lockdowns, the percentage of respondents experiencing mental distress underwent a staggering increase of 291 % for natives and 316 % for immigrants when compared to reliable pre-pandemic figures. Secondly, both before and after the COVID crisis, the unconditional differences between immigrants and natives were negligible and not statistically significant. This suggests a reasonably integrated immigrant population as shown by the convergence of emotional wellbeing between these two groups regardless of general contextual stressors. We now move to estimate net differentials in emotional wellbeing between respondents of immigrant and native origin (Table A3 in the Appendix provides the estimates from all our remaining models). There are two obvious controls that should be taken into consideration: age and access to quality housing. Regarding age, immigrants are younger than natives in Spain, 37 years of age vs 45 years of age on average (Spanish Statistical Office, 2022). Regarding housing, the living conditions of immigrants and natives differ in crucial aspects related to the lower average income and lower access to quality housing among immigrants. It has been shown that the emotional cost of confinement in Spain was higher for both young people (who also suffered a higher psychiatric morbidity) and for people living in poorer housing conditions (Jacques-Aviñó et al., 2020). It is therefore considered critical to take these two factors into account. To do so, we re-estimate the first graph adjusting for the effect of age and the square meters per capita of the household in which respondents spent time in confinement when they were interviewed, which we use as a proxy for housing quality. Finally, sex is an obvious control to add in light of the average poorer mental wellbeing of women under normal circumstances (Xiong et al., 2020). During the pandemic, many women (especially immigrant women) continued to care for the elderly and sick, exposing themselves to the risk of infection. Those working in the informal economy faced extreme vulnerability. The lack of family support for childcare, particularly when schools were closed, may also have had a negative impact on women’s mental health (Diego-Cordero et al., 2022; Ferra-Ferrer, 2020; Thibaut and Wijngaarden-Cremers, 2020). Our results (see Table A3 in the Appendix) support the assertion presented in the literature that women were at greater psychological risk during COVID-19; however, no significant difference is observed between immigrant and native-born women (see Graph 5 in the Appendix).
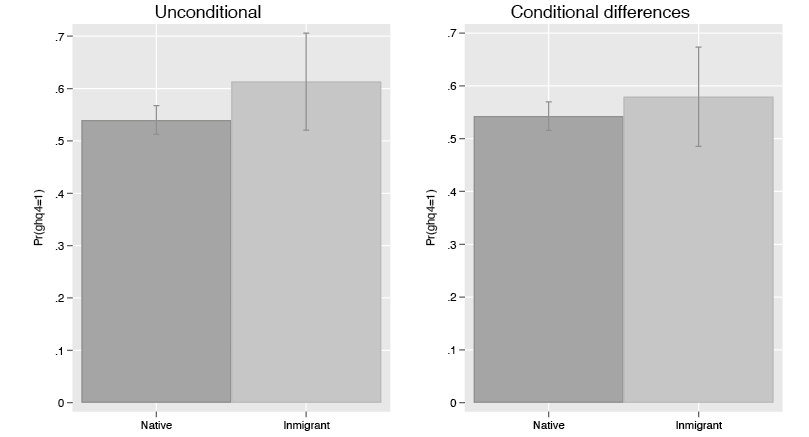
Adjusting for the selected controls confirms the robustness of our previous findings. The chart illustrates that 54.4 % of the native population in Madrid was at risk of emotional distress, compared to 57.9 % of the immigrant population. Notably, more than half of the respondents in our survey exhibited signs of compromised mental wellbeing during the harshest period of lockdown, which imposed severe restrictions on mobility. In other words, there is no empirical basis to conclude that the emotional reactions of immigrants and natives differed under lockdown. This finding highlights the emotional resilience of the immigrant population, considering obvious differences in social stratification by place of birth and structural socioeconomic vulnerability. The convergence necessitates a sound rejection of both H1 and H2.
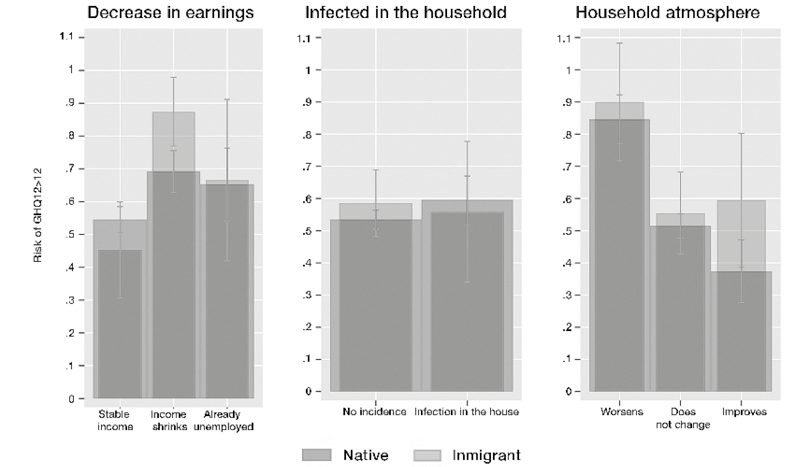
However, despite convergence, immigrants and natives may have responded differently to the unforeseen and worsening conditions that rapidly emerged as the individual and societal evolution of lockdowns worsened. For the testing of H3-H5 we need to explore how the emotional burden of three types of unexpected events was distributed: 1) experiencing a decrease in earnings due to shifting labour conditions; 2) the incidence of the disease in the household; and 3) the evolution of household atmosphere during the lockdown. To do so, we add to our model specification two-way interactions between each of three key additional stressors and immigrant status. Graph 3 summarizes the main results and, again, Table A2 in the Appendix presents the estimates and model details.
This visual summary of results suggests that the most consequential threat to immigrants’ psychological wellbeing during the pandemic and the confinements was the economic shutdown. The first Panel in Graph 3 shows how immigrant and native respondents’ psychological morbidity reacted to experiencing a decrease in earnings due to shifting labor conditions resulting from the abrupt interruption of economic activity during lockdowns. Previous evidence has already shown that respondents with low incomes and precarious jobs, more subject to changing economic circumstances during the lockdown, were more at risk of developing mental disorders (Ramírez et al., 2021; Parrado-González and León-Jariego, 2020). Shrinking incomes had more acute consequences for immigrants who, on average, have weaker support networks than natives. Specifically, our analysis reveals that the immigrant population at risk of psychological distress, as indicated in our study, was 18.0 percentage points higher than that of natives (87.4 % for immigrants and 69.2 % for natives). It is known that immigrants in Spain concentrate in segments of the secondary labour market and jobs that require in-person presence and direct interaction with clients or beneficiaries, such as in construction and caregiving (Rubio, 2020; Mahía, 2022), and are over-represented in the informal economy (Repič, 2010). This explains why their income was more likely to shrink during the fierce restrictive measures taken that greatly reduced economic activity. Our findings provide a sound confirmation of H3, which theorizes that immigrant economic vulnerability has different sources than native vulnerability, although the average level of instability and poor employment conditions are shared with many natives. This has to do with the limited ability of immigrants to share resources to confront the unexpected or to maintain their economic responsibilities toward their family of origin. Finally, note that those who were unemployed before the Pandemic and those whose working conditions did not lead to shrinking revenues show a similar behaviour across immigrant status.
While the greater psychological vulnerability of immigrants compared to natives during economic crises has been previously documented (Robert et al., 2014), our study is, to the best of our knowledge, the first to consider other unexpected stressors. We have examined how immigrants and natives reacted to the incidence of the Covid at home, a situation that could be a trigger for stress dynamics. H4 stated that when exposed to the infection, immigrant households would have a stronger negative emotional reaction than natives because of their likely imperfect knowledge of the healthcare system and, in some cases, more limited access to it. The results reject this scenario and show that immigrants and natives reacted similarly to the event of having to isolate members of the household due to infections or the suspicion of being infected. We can, thus, conclude that the differences in loss of mental wellbeing between immigrants and natives do not seem to be due to differences in the incidence of illness or coping with it, but, as we will see below, to other contextual factors. Lastly, the pandemic had a huge impact on family organization and cohabitation in many households. We looked at how immigrants and natives were affected by the household atmosphere and family relationships under the extreme conditions imposed (Günther-Bel et al., 2020), as expected from H5. The necessity to spend time under the same roof and the disruptions to daily life could be seen as potential triggers of family conflict. Although the highest levels of psychological risk are found among those who reported that cohabitation in their family had worsened (84.6 % of natives and 90 % of immigrants), differences across immigrant status are not statistically different.
Robustness checks
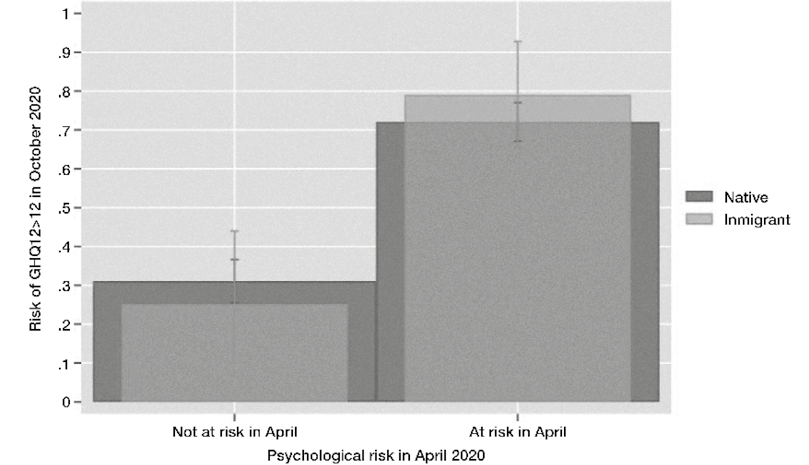
Complementary tests were conducted to confirm the robustness of our results to alternative specifications, yielding no changes in the reported results. Controlling for the presence of elderly individuals in the household (considered an additional stressor due to their vulnerability to COVID) or adjusting for household type (which incorporates single-person households into the analyses concerning family atmosphere) did not alter our conclusions. Utilizing fixed effects instead of random terms to model individual clustering in space did not distort our conclusions either. In addition, employing linear probability models upheld all of our findings. Lastly, we replicated our baseline analyses with data from the second wave of our Madrid Covid Household Panel, the fieldwork for which was carried out in October, 2020, confirming the pattern of strong convergence between immigrants and natives in their likelihood of being under psychological risk. Graph 4 provides a visual summary of this robustness check (detailed estimates are presented in Table A3: Model 6, which also controls for baseline score in GHQ12 in April 2020).
Discussion
Research into social vulnerability and disadvantage is increasingly centred on understanding individual experiences that predispose individuals to different degrees of success. It would not be an exaggeration to state that emotional wellbeing is a fundamental prerequisite for achieving optimal outcomes in education and the labour market. Research on immigrant integration must incorporate this perspective.
Our analysis delivers both positive and negative news regarding the integration of immigrants in Madrid, and potentially the rest of Spain if the observed pattern holds true across the country. The overarching message is that differences in the mental wellbeing of immigrants and natives consistently remain negligible, under both normal circumstances (back in 2017) and the intensely stressful conditions imposed by the April 2020 lockdowns. Hence, our findings reveal immigrants to be a resilient population that, just as the general population, encountered substantial psychological burdens during the spring 2020 lockdowns. This is noteworthy, given that immigrants typically face significantly more challenging daily circumstances compared to natives, as suggested by integration literature, which reveals immigrants to be a group that is particularly vulnerable to external shocks. As indicated by our models, the occurrence of illness within the household and the dynamics of family coexistence during lockdowns did not differentially affect respondents in Madrid based on their immigrant status. At least within this lesser-explored dimension of integration, namely mental wellbeing, our immigrant population demonstrated a notable convergence with the native population. This trend, undoubtedly a desirable outcome, warrants a positive reception.
Importantly, there is one crucial aspect in which immigrants were shown to be significantly more psychologically vulnerable than the Spanish-born. Those who lived in households that experienced income loss suffered a much higher risk of suffering psychological distress than the native-born. Specifically, among this group the percentage at risk of psychological distress increased some 18 percentage points more for immigrants than for natives (69.7 % for natives and 87.7 for migrants). This greater psychological vulnerability of economic immigrants to financial stress confirms findings from other countries where similar studies have been carried out (Choudhari, 2020; Garcini et al., 2016, 2022).
The implications for integration research are critical. Economic precariousness is the key factor affecting immigrant integration, possibly predisposing immigrants and natives to face adverse circumstances differently. There are multiple reasons why income loss could be more harmful for immigrants than for natives. First, the loss of income in lower-income households is more difficult to manage than in middle- and high-income households, among other things because of the potential for available savings to aid in coping with unexpected contingencies in the latter households. Moreover, immigrants may have less well-developed social networks and fewer other resources to support them in case of need. Further research focusing on this matter, delving into the interplay among social support, socioeconomic status, and immigrant status, is indispensable for gaining a more comprehensive understanding of the potential risks immigrants might encounter during future social crises. Additionally, it would be worthwhile to investigate the long-term effects of COVID-19 through longitudinal studies, as it appears that the pandemic’s impact on mental health has, in many cases, not been temporary (Pennix et al., 2022). A better understanding of the issues discussed here would allow the development of future ad-hoc public policies during times of crisis, for example, activating economic support networks specifically aimed at particularly vulnerable groups (such as immigrants). These kinds of initiatives would be aimed not only at maintaining immigrants’ material conditions but also at protecting their mental health.
Limitations of the current research
While our conclusions remain robust across time, contexts, and various datasets, it is important to acknowledge several significant limitations within this study. Our focus is solely on the determinants of psychological risk among immigrants and not on ethnicity, as disentangling ethnic ascriptions proved to be unfeasible. Limitations in the survey questionnaire hinder our ability to fully isolate the impacts of essential variables like household income, per capita earnings, and migration-related factors such as time since migration. Furthermore, the influence of personality traits are not controlled for, thereby restricting the integration of self-selection factors into our immigration-focused research. Future research should overcome these limitations and foster the inclusion of epidemiological indicators of wellbeing in mainstream population surveys.
Bibliography
Acharya, Shiva R.; Moon, Deog H.; Chun, Jin Ho and Shin, Yong Chul (2022). “COVID-19 and Mental Health: Anxiety Disorders among Immigrants Due to COVID-19 Outbreak in South Korea”. The International Journal of Psychiatry in Medicine, 57(4): 323-337. doi: 10.1177/00912174211042695
Achotegui, Joseba (2009). “Migración y Salud Mental. El Síndrome del Inmigrante con Estrés Crónico y Múltiple (Síndrome de Ulises)”. Zerbitzuan, 46(163): 163-171. doi: 10.1016/s0304-4858(09)74665-7
Achotegui, Joseba (2017). “Acerca de la Psiquiatrización y el Sobrediagnóstico de los Traumas en los Inmigrantes y Refugiados”. Temas de Psicoanálisis, 13: 1-14.
Adhikari, Ramesh; Jampaklay, Aree and Chamratrithirong, Aphichat (2011). “Impact of Children’s Migration on Health and Health Care-Seeking Behavior of Elderly Left Behind”. BMC Public Health, 11(143). doi: 10.1186/1471-2458-11-143
Agius Vallejo, Jody and Keister, Lisa A. (2020). “Immigrants and Wealth Attainment: Migration, Inequality, and Integration”. Journal of Ethnic and Migration Studies, 46(18): 3745-3761. doi: 10.1080/1369183x.2019.1592872
Antecol, Heather and Bedard, Kelly (2006). “Unhealthy Assimilation: Why Do Immigrants Converge to American Health Status Levels?”. Demography, 43(2): 337-360. doi: 10.1353/dem.2006.0011
Arora, Sanjana; Bø, Bodil; Tjoflåt, Ingrid and Eslen-Ziya, Hande (2022). “Immigrants in Norway: Resilience, Challenges, and Vulnerabilities in Times of COVID-19”. Journal of Migration and Health, 5: 100089. doi: 10.1016/j.jmh.2022.100089
Bak-Klimek, Anna; Karatzias, Thanos; Elliott, Lawrie and Maclean, Rory (2015). “The Determinants of Well-Being among International Economic Immigrants: A Systematic Literature Review and Meta-Analysis”. Applied Research in Quality of Life, 10: 161–188. doi: 10.1007/s11482-013-9297-8
Baksheev, Gennady N.; Robinson, Jo; Cosgrave, Elizabeth M.; Baker, Kathryn and Yung, Alison R. (2011). “Validity of the 12-Item General Health Questionnaire (GHQ-12) in Detecting Depressive and Anxiety Disorders among High School Students”. Psychiatry Research, 187(1-2): 291-296. doi: 10.1016/j.psychres.2010.10.010
Banal, Rakesh; Thappa, Jagdish; Shah, H. U.; Hussain, Arshid; Chowhan, Abhishek; Kaur, Harneet; Bharti, Mala and Thappa, Sushant (2010). “Psychiatric Morbidity in Adult Kashmiri Migrants Living in a Migrant Camp at Jammu”. Indian Journal of Psychiatry, 52(2): 154. doi: 10.4103/0019-5545.64597
Bell, Truda; Watson, Margaret; Sharp, Deborah; Lyons, Ita and Lewis, Glyn (2005). “Factors Associated with Being a False Positive on the General Health Questionnaire”. Social Psychiatry and Psychiatric Epidemiology, 40: 402-407. doi: 10.1007/s00127-005-0881-6
Bover, Olympia; Hospido, Laura and Villanueva, Ernesto (2018). Encuesta de Competencias Financieras (ECF) 2016: Principales Resultados. CNMV, Comisión Nacional del Mercado de Valores. doi: 10.2139/ssrn.3396964
Brady, David (2019). “Theories of the Causes of Poverty”. Annual Review of Sociology, 45: 155-175.
Breslau, Joshua (2011). “Migration and Mental Health. Edited by D. Bhugra and S. Gupta. Cambridge University Press: New York. (2011)”. Psychological Medicine, 41(2233). doi: 10.1017/S0033291711001346
Brown, Sarah; Harris, Mark N.; Srivastava, Preety and Taylor, Karl (2018). “Mental Health and Reporting Bias: Analysis of the GHQ-12”. IZA Discussion Papers, 11771: 1-43. doi: 10.2139/ssrn.3249885
Buitrago, Ramírez, Francisco; Ciurana Misol, Ramón; Fernández Alonso, María del Carmen and Tizón García, Jorge Luis (2021). “Repercusiones de la Pandemia de la COVID-19 en la Salud Mental de la Población General. Reflexiones y Propuestas”. Atención Primaria, 53(7). doi: 10.1016/j.aprim.2021.102143
Casado, Ramón Mahía (2022). “Medición de la Integración de la Población Extranjera en el Mercado Laboral Español”. Mediterráneo Económico, 36: 19-38.
Cebolla Boado, Héctor and Aratani, Yumiko (2020). “Determinantes del Estrés Psicológico No Específico entre los Adolescentes Latinoamericanos en Madrid”. Revista Española de Investigaciones Sociológicas, 169: 41-62. doi: 10.5477/cis/reis.169.41
Cebolla Boado, Héctor and González Ferrer, Amparo (2022). “The Impact of Physical Separation from Parents on the Mental Wellbeing of the Children of Migrants”. Journal of Ethnic and Migration Studies, 48(10): 2436-2454. doi: 10.1080/1369183x.2021.1935670
Choudhari, Ranjana (2020). “COVID-19 Pandemic: Mental Health Challenges of Internal Migrant Workers of India”. Asian Journal of Psychiatry, 54: 102254. doi: 10.1016/j.ajp.2020.102254
Choy, B.; Arunachalam, K.; Gupta, S.; Taylor, M. and Lee, A. (2021). “Systematic Review: Acculturation Strategies and Their Impact on the Mental Health of Migrant Populations”. Public Health in Practice, 2: 100069. doi: 10.1016/j.puhip.2020.100069
Dhadda, Amrit and Greene, Giles (2018). “`The Healthy Migrant Effect´ for Mental Health in England: Propensity-Score Matched Analysis Using the EMPIRIC Survey”. Journal of Immigrant and Minority Health, 20: 799-808. doi: 10.1007/s10903-017-0570-z
Diego-Cordero, Rocío; Tarriño Concejero, Lorena; Lato Molina, María A. and García-Carpintero Muñoz, María A. (2022). “COVID-19 and Female Immigrant Caregivers in Spain: Cohabiting during Lockdown”. European Journal of Women’s Studies, 29(1): 123-139. doi: 10.1177/13505068211017577
Doàn, Lan; Chong, Stella K.; Misra, Supriya; Kwon, Simona C. and Yi, Stella S. (2021). “Immigrant Communities and COVID-19: Strengthening the Public Health Response”. American Journal of Public Health, 111(S3): S224-S231. doi: 10.2105/AJPH.2021.306433
Ekwonye, Angela U.; Ezumah, Bellarmine A. and Nwosisi, Ngozi (2021). “Meaning in Life and Impact of COVID-19 Pandemic on African Immigrants in the United States”. Wellbeing, Space and Society, 2: 100033. doi: 10.1016/j.wss.2021.100033
Elshahat, Sarah; Moffat, Tina and Newbold, K. Bruce (2022). “Understanding the Healthy Immigrant Effect in the Context of Mental Health Challenges: A Systematic Critical Review”. Journal of Immigrant and Minority Health, 24(6): 1564-1579. doi: 10.1007/s10903-021-01313-5
Endale, Tarik; St Jean, Nicole and Birman, Dina (2020). “COVID-19 and Refugee and Immigrant Youth: A Community-Based Mental Health Perspective”. Psychological Trauma: Theory, Research, Practice, and Policy, 12(S1). doi: 10.1037/tra0000875
Enriquez, Laura E.; Morales, Alberto E.; Rodriguez, Victoria E.; Chavarria, Karina and Ro, Annie (2022). “Mental Health and COVID-19 Pandemic Stressors Among Latina/o/x College Students with Varying Self and Parental Immigration Status”. Journal of Racial and Ethnic Health Disparities, 10(1): 282-295. doi: 10.1007/s40615-021-01218-x
Escudero-Castillo, Israel; Mato-Díaz, Fco. Javier and Rodríguez-Álvarez, Ana (2023). “Psychological Well-Being during the COVID-19 Lockdown: Labour Market and Gender Implications”. Applied Research in Quality of Life, 18(1): 71-91. doi: 10.1007/s11482-022-10113-4
Ferrer-Perez, Victoria (2020). “Coping with the COVID-19 Pandemic and Its Consequences from the Vantage Point of Feminist Social Psychology”. International Journal of Social Psychology, 35(3): 639-646. doi: 10.1080/02134748.2020.1783839
Florence, Thibaut and Wijngaarden-Cremers, Patricia J. van (2020). “Women’s Mental Health in the Time of COVID-19 Pandemic”. Frontiers in Global Women’s Health, 1: 588372. doi: 10.3389/fgwh.2020.588372
García, Rodrigo Jiménez (2020). “COVID-19 en la Ciudad de Madrid y Vulnerabilidad. Análisis de las Dos Primeras Olas”. Methods, 95: e1-10.
Garcini, Luz M.; Murray, Kate; Zhou, Anne; Klonoff, Elizabeth; Myers, Mark G. and Elder, John P. (2016). “Mental Health of Undocumented Immigrant Adults in the United States: A Systematic Review of Methodology and Findings”. Journal of Immigrant & Refugee Studies, 14(1): 1-25. doi: 10.1080/15562948.2014.998849
Garcini, Luz M.; Rosenfeld, Jason; Kneese, Garrett; Bondurant, Ruth G. and Kanzler, Kathryn E. (2022). “Dealing with Distress from the COVID-19 Pandemic: Mental Health Stressors and Coping Strategies in Vulnerable Latinx Communities”. Health & Social Care in the Community, 30(1): 284-294. doi: 10.1111/hsc.13402
Garrido, Rocío; Paloma, Virginia; Benítez, Isabel; Skovdal, Morten; Verelst, An and Derluyn, Ilse (2023). “Impact of COVID-19 Pandemic on the Psychological Well-Being of Migrants and Refugees Settled in Spain”. Ethnicity & Health, 28(2): 257-280. doi: 10.1080/13557858.2022.2035692
Goldberg, David P.; Gater, Richard; Sartorius, Norman; Ustun, Tevfik B.; Piccinelli, Marina; Gureje, Oye and Rutter, Cindy (1997). “The Validity of Two Versions of the GHQ in the WHO Study of Mental Illness in General Health Care”. Psychological Medicine, 27(1): 191–97. doi: 10.1017/s0033291796004242
Griffith, Gareth J. and Jones, Kelvyn (2019). “Understanding the Population Structure of the GHQ-12: Methodological Considerations in Dimensionally Complex Measurement Outcomes”. Social Science & Medicine, 243: 112638. doi: 10.1016/j.socscimed.2019.112638
Günther-Bel, Cristina; Vilaregut, Anna; Carratala, Eduard; Torras-Garat, Sonia and Pérez-Testor, Carles (2020). “A Mixed-Method Study of Individual, Couple, and Parental Functioning during the State-Regulated COVID-19 Lockdown in Spain”. Family Process, 59(3): 1060-1079. doi: 10.1111/famp.12585
Hacker, Karen; Anies, Maria; Folb, Barbara L. and Zallman, Leah (2015). “Barriers to Health Care for Undocumented Immigrants: A Literature Review”. Risk Management and Healthcare Policy, 175-83. doi: 10.2147/RMHP.S70173
Hasan, Siti I.; Yee, Anne; Rinaldi, Ariyani; Azham, Adlina A.; Mohd Hairi, Farizah and Amer Nordin, Siddiq (2021). “Prevalence of Common Mental Health Issues among Migrant Workers: A Systematic Review and Meta-Analysis”. PLOS ONE, 16(12): e0260221. doi: 10.1371/j.pone.0260221
He, Xuesong and Wong, Daniel F. (2013). “A Comparison of Female Migrant Workers’ Mental Health in Four Cities in China”. The International Journal of Social Psychiatry, 59(2): 114-122. doi: 10.1177/0020764011423467
Hendriks, Martijn and Bartram, David (2019). “Bringing Happiness into the Study of Migration and Its Consequences: What, Why, and How?”. Journal of Immigrant & Refugee Studies, 17(3): 279-298. doi: 10.1080/15562948.2018.1458169
Hernández Plaza, Sonia ; Pozo Muñoz, Carmen; Alonso Morillejo, Enrique and Martos Méndez, María J. (2005). “Estructura y Funciones del Apoyo Social en un Colectivo de Inmigrantes Marroquíes”. Anales de Psicología, 21(2): 304-315. doi: 10.1016/j.rlp.2014.07.002
INE (2022). Estadística del Padrón Continuo. Available at : https://www.ine.es/jaxi/Tabla.htm?path=/t20/e245/p08/l0/&file=01007.px&L=0
Jacques-Aviñó, Constanza; López-Jiménez, Tomàs; Medina-Perucha, Laura; de Bont, Jeroen; Queiroga Gonçalves, Alessandra; Duarte-Salles, Talita and Berenguera, Anna (2020). “Gender-Based Approach on the Social Impact and Mental Health in Spain during COVID-19 Lockdown: A Cross-Sectional Study”. BMJ Open, 10(11): e044617.
Jariego, Isidro Maya (2009). “Mallas de Paisanaje: El Entramado de Relaciones de los Inmigrantes”. Redes: Revista Hispana Para El Análisis de Redes Sociales, 17(13): 273–303. doi: 10.5565/rev/redes.385
Jarrín, Inma; García-Fulgueiras, Ana; Ibánez-Rojo, Vicente; Alvarez, Débora; García-Pina, Rocío; Fernández-Liria, Alberto; García-Ortúzar, Visitación; Díaz, Domingo; Rodríguez-Arenas, Maria Ángeles and Mazarrasa, Lucía (2013). “Absence of Protective Ethnic Density Effect on Ecuadorian Migrants’ Mental Health in a Recent Migration Setting: A Multilevel Analysis”. Social Psychiatry and Psychiatric Epidemiology, 48: 95-103. doi 10.1007/s00127-012-0523-8
Kessler, Ronald C.; Andrews, Gavin; Colpe, Lisa J.; Hiripi, E.; Mroczek, Daniel K.; Normand, Sharon-Lise T.; Walters, Ellen E. and Zaslavsky, Alan M. (2002). “Short Screening Scales to Monitor Population Prevalences and Trends in Non-Specific Psychological Distress”. Psychological Medicine, 32(6): 959-976. doi: 10.1017/S0033291702006074
Kindler, Marta; Ratcheva, Vesselina and Piechowska, Maria (2015). “Social Networks, Social Capital y Migrant Integration at Local Level. European Literature Review”. Institute For Research Into Superdiversity, 6: 1-22.
Lundin, Andreas; Hallgren, M.; Theobald, Holger; Hellgren, Carina and Torgén, Margareta (2016). “Validity of the 12-Item Version of the General Health Questionnaire in Detecting Depression in the General Population”. Public Health, 136: 66-74. doi: 10.1016/j.puhe.2016.03.005
Maggi, Stefania; Ostry, Aleck; Callaghan, Kristy; Hershler, Ruth; Chen, Lisa; D’Angiulli, Amedeo and Hertzman, Clyde (2010). “Rural-Urban Migration Patterns and Mental Health Diagnoses of Adolescents and Young Adults in British Columbia, Canada: A Case-Control Study”. Child and Adolescent Psychiatry and Mental Health, 4(13). doi: 10.1186/1753-2000-4-13
Merchant, Emily K. (2021). Assessing the Demographic Consequences of the COVID-19 Pandemic. In: L. MacKellar and R. Friedman (eds). Covid-19 and the Global Demographic Research Agenda. New York: Population Council. doi: 10.31899/pdr1.1007
Mood, Carina; Jonsson, Jan O. and Brolin Låftman, Sara (2016). “The Mental Health Advantage of Immigrant-Background Youth: The Role of Family Factors”. Journal of Marriage and Family, 79(2): 419-436. doi: 10.1111/jomf.12340
Ngo, Thoai and Psaki, Stephanie (2021). Rethinking the Role of Demographers in Times of Crisis». In: L. MacKellar and R. Friedman (eds). Covid-19 and the Global Demographic Research Agenda. New York: Population Council. doi: 10.31899/pdr1.1005
Odegaard, Ornulv (1932). “Emigration and Insanity: A Study of Mental Disease among the Norwegian-Born Population of Minnesota”. Acta Psychiatrica Scandinavica, 4: 1-206.
Parella Rubio, Sònia (2020). “El Sector del Trabajo del Hogar y de Cuidados en España en Tiempos de COVID-19”. Anuario CIDOB de la Inmigración, 101-114. doi: 10.24241/anuariocidobinmi.2020.102
Parrado-González, Alberto and León-Jariego, José C. (2020). “COVID-19: Factores Asociados al Malestar Emocional y Morbilidad Psíquica en Población Española”. Revista Española de Salud Pública, 94(8): 202006058. doi: 10.21203/rs.3.rs-49587/v1
Penninx, Brenda; Benros, Michael E.; Klein, Robyn S. and Vinkers, Christiaan H. (2022). “How COVID-19 Shaped Mental Health: From Infection to Pandemic Effects”. Nature Medicine, 28(10): 2027-2037. doi: 10.1038/s41591-022-02028-2
Repič, Jaka (2010). “Migration, Informal Economy and Social Exclusion in Spain”. Studia Ethnologica Croatica, 22: 165-186.
Riosmena, Fernando; Kuhn, Randall and Jochem, Warren C. (2017). “Explaining the Immigrant Health Advantage: Self-Selection and Protection in Health-Related Factors among Five Major National-Origin Immigrant Groups in the United States”. Demography, 54(1): 175-200. doi: 10.1007/s13524-016-0542-2
Rivera, Berta; Casal, Bruno and Currais, Luis (2016). “The Healthy Immigrant Effect on Mental Health: Determinants and Implications for Mental Health Policy in Spain”. Administration and Policy in Mental Health and Mental Health Services Research, 43(4): 616-627. doi: 10.1007/s10488-015-0668-3
Robert, Gemma; Martínez, José M.; García, Ana M.; Benavides, Fernando G. and Ronda, Elena (2014). “From the Boom to the Crisis: Changes in Employment Conditions of Immigrants in Spain and Their Effects on Mental Health”. The European Journal of Public Health, 24(3): 404-409. doi: 10.1093/eurpub/cku020
Rocha, Kátia B.; Pérez, Katherine; Rodríguez-Sanz, Maica; Borrell, Carme and Obiols, Jordi E. (2011). “Propiedades Psicométricas y Valores Normativos del General Health Questionnaire (GHQ-12) en Población General Española”. International Journal of Clinical and Health Psychology, 11(1): 125-139. doi: 10.1007/s00127-012-0474-0
Rodrigo, Maria F.; Molina, J. Gabriel; Losilla, Josep-Maria; Vives, Jaume and Tomás, José M. (2019). “Method Effects Associated with Negatively and Positively Worded Items on the 12-Item General Health Questionnaire (GHQ-12): Results from a Cross-Sectional Survey with a Representative Sample of Catalonian Workers”. BMJ Open, 9(11): e031859. doi: 10.1136/bmjopen-2019-031859
Salinero-Fort, Miguel Á.; del Otero-Sanz, Laura; Martín-Madrazo, Carmen; de Burgos-Lunar, Carmen; Chico-Moraleja, Rosa M.; Rodés-Soldevila, Berta; Jiménez-García, Rodrigo; Gómez-Campelo, Paloma and Health & Migration Group (2011). “The Relationship between Social Support and Self-Reported Health Status in Immigrants: An Adjusted Analysis in the Madrid Cross Sectional Study”. BMC Family Practice, 12: 1-9. doi: 10.1186/1471-2296-12-46
Sarasa, Sebastià; Navarro-Varas, Lara and Porcel, Sergio (2016). “Clase Social y Privación Material entre los Inmigrantes de Países Pobres en Cataluña/Social Class and Material Deprivation in Immigrants from Poor Countries Residing in Catalonia”. Revista Española de Investigaciones Sociológicas, 156: 117-140. doi: 10.5477/cis/reis.156.117
Shen, Jing and Bartram, David (2021). “Fare Differently, Feel Differently: Mental Well-Being of UK-Born and Foreign-Born Working Men during the COVID-19 Pandemic”. European Societies, 23: S370-83. doi: 10.1080/14616696.2020.1826557
Snijders, Tom A. B. and Bosker, Roel J. (2012). Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling. UK: Sage.
Stillman, Steven; Gibson, John and McKenzie, David (2012). “The Impact of Immigration on Child Health: Experimental Evidence from a Migration Lottery Program”. Economic Inquiry, 50(1): 62-81. doi: 10.1111/j.1465-7295.2009.00284.x
Teruya, Stacey A. and Bazargan-Hejazi, Shahrzad (2013). “The Immigrant and Hispanic Paradoxes: A Systematic Review of Their Predictions and Effects”. Hispanic Journal of Behavioral Sciences, 35(4): 486-509. doi: 10.1177/0739986313499004
Turra, Cassio M. and Elo, Irma T. (2008). “The Impact of Salmon Bias on the Hispanic Mortality Advantage: New Evidence from Social Security Data”. Population Research and Policy Review, 27: 515-30. doi: 10.1007/s11113-008-9087-4
Williams, Paul and Goldberg, David P. (1988). A User’s Guide to the General Health Questionnaire. Berkshire: NFER, Nelson.
Xiong, Jiaqi; Lipsitz, Orly; Nasri, Flora; Lui, Leanna M.; Gill, Hartej; Phan, Lee; Chen-Li, David; Iacobucci, Michelle; Ho, Roger and Majeed, Amna (2020). “Impact of COVID-19 Pandemic on Mental Health in the General Population: A Systematic Review”. Journal of Affective Disorders, 277: 55-64. doi: 10.1016/j.jad.2020.08.001
Appendix
Table A1. Summary or variables and descriptive information
|
|
N
|
Mean
|
SD
|
|
Components
of GHQ12
|
Have you been able to concentrate well on what you were doing?
|
197
|
1.7
|
0.95
|
|
Have your worries made you lose a lot of sleep?
|
204
|
1.4
|
1.1
|
|
Have you felt that you are playing a useful role in life?
|
181
|
1.2
|
0.83
|
|
Have you felt capable of making decisions?
|
196
|
1.1
|
0.7
|
|
Have you felt constantly overwhelmed and tense?
|
206
|
1.5
|
1.1
|
|
Have you had the feeling that you cannot overcome your difficulties?
|
196
|
0.8
|
0.93
|
|
Have you been able to enjoy your normal daily activities?
|
194
|
1.7
|
0.93
|
|
Have you been able to adequately cope with your problems?
|
194
|
1.2
|
0.66
|
|
Have you felt unhappy or depressed?
|
201
|
1.3
|
0.99
|
|
Have you lost confidence in yourself?
|
203
|
0.44
|
0.79
|
|
Have you thought that you are a worthless person?
|
198
|
0.3
|
0.73
|
|
Do you feel reasonably happy considering all the circumstances?
|
198
|
1.2
|
0.69
|
|
GHQ12 synthetic
|
|
137
|
0.59
|
0.49
|
|
Immigrant
|
|
206
|
0.11
|
0.31
|
|
Female
|
|
206
|
0.61
|
0.49
|
|
Age
|
|
206
|
45
|
24
|
|
House m2 pc
|
|
124
|
47
|
30
|
|
Education
|
Primary or less
|
132
|
0.21
|
0.41
|
|
Secondary
|
132
|
0.38
|
0.49
|
|
Vocational
|
132
|
0.14
|
0.34
|
|
University
|
132
|
0.27
|
0.45
|
|
Evolution of earnings due to shifting labor conditions
|
Stable income
|
666
|
0.67
|
0.46
|
|
Decreasing income
|
233
|
0.23
|
0.42
|
|
Already unemployed before April 2020
|
84
|
0.08
|
0.28
|
|
Incidence of Covid
|
|
206
|
0.16
|
0.36
|
|
Atmosphere
|
Worsens
|
134
|
0.16
|
0.36
|
|
Does not change
|
134
|
0.69
|
0.46
|
|
Improves
|
134
|
0.15
|
0.36
|
Table A2. Logistic models on GHQ12>12
|
ENS 2017
|
Covid Madrid 2020
|
|
Immigrant (ref.: natives)
|
0.062
|
0.30
|
|
(0.16)
|
(0.21)
|
|
Constant
|
-1.48*
|
0.16*
|
|
(0.062)
|
(0.057)
|
|
N
|
2008
|
1360
|
|
Chi2
|
0.15
|
2.11
|
Legend: Standard errors in parentheses.
* p<0.05.
Source: By the authors.
Table A3. Binary logistic hierarchical models on GHQ12>12
|
Dependent variable
|
|
Risk in April 2020
|
Risk in October 2020
|
|
|
(1)
|
(2)
|
(3)+
|
(4)++
|
(5)
|
(6)+++
|
|
Immigrant
(ref. natives)
|
|
0.30
|
0.15
|
-0.38
|
0.21
|
0.51
|
-0.30
|
|
|
(0.21)
|
(0.21)
|
(0.32)
|
(0.23)
|
(1.10)
|
(0.54)
|
|
Female (ref. male)
|
|
|
0.25*
|
0.25
|
0.25*
|
0.15
|
0.69*
|
|
|
|
(0.11)
|
(0.13)
|
(0.11)
|
(0.14)
|
(0.16)
|
|
Age
|
|
|
-0.019*
|
-0.0098
|
-0.018*
|
-0.018*
|
0.0028
|
|
|
|
(0.0040)
|
(0.0062)
|
(0.0040)
|
(0.0050)
|
(0.0060)
|
|
Per capita M2
|
|
|
-0.00014
|
0.0018
|
-0.0039
|
-0.0015
|
0.0023
|
|
|
|
(0.0020)
|
(0.0032)
|
(0.0024)
|
(0.0044)
|
(0.0031)
|
|
Education
(ref. is primary or less)
|
Secondary
|
|
0.21
|
0.62
|
0.22
|
0.26
|
0.043
|
|
|
|
(0.25)
|
(0.56)
|
(0.25)
|
(0.36)
|
(0.41)
|
|
Vocational
|
|
0.060
|
0.57
|
0.059
|
0.21
|
-0.26
|
|
|
|
(0.28)
|
(0.57)
|
(0.28)
|
(0.39)
|
(0.45)
|
|
University
|
|
0.35
|
1.07
|
0.36
|
0.53
|
-0.27
|
|
|
|
(0.25)
|
(0.56)
|
(0.25)
|
(0.36)
|
(0.40)
|
|
Impact on income (ref. is no changes)
|
Income shrinks
|
|
|
0.64*
|
|
|
|
|
|
|
|
(0.18)
|
|
|
|
|
Respondent already unemployed
|
|
|
0.46
|
|
|
|
|
|
|
|
(0.27)
|
|
|
|
|
Interaction
|
Immigrant*income shrinks
|
|
|
1.53*
|
|
|
|
|
|
|
|
(0.60)
|
|
|
|
|
Immigrant*respondent already unemployed
|
|
|
0.44
|
|
|
|
|
|
|
|
(0.70)
|
|
|
|
|
Hhld members infected
|
|
|
|
|
0.26
|
|
|
|
|
|
|
|
(0.17)
|
|
|
|
Interaction
|
Migrant # household members isolated
|
|
|
|
-0.37
|
|
|
|
|
|
|
|
(0.55)
|
|
|
|
Hhold atmosphere (ref. is worsens)
|
Does not change
|
|
|
|
|
-1.70*
|
|
|
|
|
|
|
|
(0.31)
|
|
|
Improves
|
|
|
|
|
-2.29*
|
|
|
|
|
|
|
|
(0.37)
|
|
|
Interaction
|
Immigrant*Does
not change
|
|
|
|
|
-0.34
|
|
|
|
|
|
|
|
(1.13)
|
|
|
Immigrant*Improves
|
|
|
|
|
0.42
|
|
|
|
|
|
|
|
(1.21)
|
|
|
Respondent already at risk in April 2020 (ref. not at risk)
|
|
|
|
|
|
|
1.84*
|
|
|
|
|
|
|
|
(0.17)
|
|
Interaction
|
Immigrant*risk in April 2020
|
|
|
|
|
|
0.70
|
|
|
|
|
|
|
|
(0.70)
|
|
Constant
|
|
0.16*
|
0.76*
|
-0.51
|
0.69*
|
2.23*
|
-1.29*
|
|
|
(0.06)
|
(0.35)
|
(0.62)
|
(0.35)
|
(0.55)
|
(0.56)
|
|
Model info.
|
N
|
1360
|
1360
|
983
|
1360
|
943
|
821
|
|
Chi2
|
2.34
|
46.6
|
40.7
|
48.6
|
72.9
|
142.6
|
Legend: Standard errors in parentheses.
* p<0.05.
Notes on analytic samples:
+ Sample in Model 3 excludes the inactive population.
++ Sample in Model 4 exclude single person households.
+++ Model 5 is estimated using the second wave of the Madrid Covid Household Panel.
Source: By the authors.